A short note of epithelial ovarian tumor (part 1: serous tumor)
General Idea
- Arise from mullerian epithelium
- Mainly described by histologic types (e.g. serous, mucinous, endometrioid), Behavior (benign, borderline, malignant), and tumor component (eg. cystadenoma, cystadenofibroma, adenofibroma)
- 2 main pathogenesis
- Low grade tumor: associated with borderline tumor and endometriosis
- High grade tumor (commonly high grade serous carcinoma) associated with cortical inclusion cyst and Serous tubal intraepithelial carcinoma (STIC)
Serous tumor
- Most common malignant ovarian tumor (40% of all cancer of ovary)
- 70% benign or borderline tumor (usually occurs at 20-45 year old), 30% malignant tumor (mean age 63 year old 2)
- Risk factors (high grade serous)3: Lower parity, Shorter duration of OC use, Longer duration of postmenopausal hormonal therapy, No history of tubal ligation, Family history of ovarian cancer (inherited germ line BRCA1 and BRCA2 -> associated with STIC)
- Molecular alteration of malignant tumor:
- Low grade serous tumor: KRAS, BRAF, or ERBB2 oncogene mutation, Wild-type TP53
- High grade serous tumor: usually have TP53 mutation with lack mutation in KRAS or BRAF, inactivation of BRCA1 and BRCA2 in 50% of cases, amplification of PIK3CA oncogene can also present 2
- gross description: oval to round, smooth glistening cyst with watery or pale yellow fluid ± small papillary excrescences (Increase papillary growth+irregularity+fixation = likely malignancy)
- Microscopic finding (Key: papillary ± psammoma body)
| Grading | Microscopic features |
|---|---|
| Benign (cystadenoma) | Uni-multi cysts lined by columnar ciliated epithelium (or non-ciliated cuboid) ± microscopic papillae |
| Borderline | Increase complexity of stromal papillae+mild nuclear atypia+Stratification of epithelium but no stromal invasion, maybe precursor for low-grade serous carcinoma |
| High grade | Complex growth pattern, infiltration, effacement of stroma, cells display marked atypia, high pleomorphism, atypical mitosis, multinucleation |
Table 1: Microscopic features of benign, borderline, and high grade serous tumors of ovary
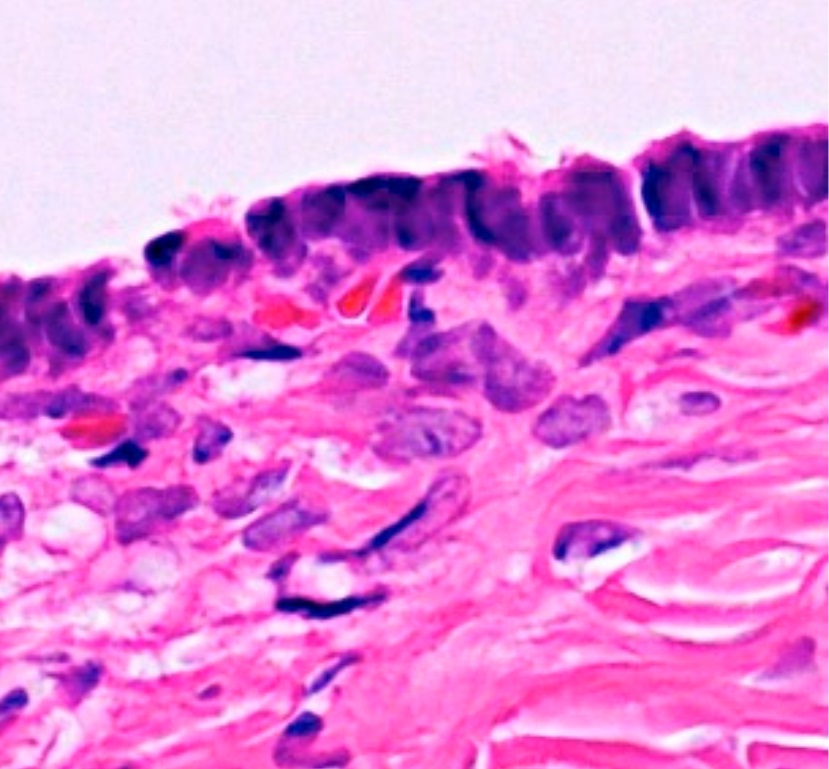 "Histopathology of serous cystadenoma" by Michiko Nagamine, and Yoshiki Mikami is licensed under CC BY 4.0.
"Histopathology of serous cystadenoma" by Michiko Nagamine, and Yoshiki Mikami is licensed under CC BY 4.0.
 "Serous carcinoma" by euthman is licensed under CC BY 2.0.
"Serous carcinoma" by euthman is licensed under CC BY 2.0.
- Prognosis assoc w/ histology and peritoneal metastasis (staging) 1
| Histologic grading | confined to ovary | With peritoneal metastasis |
|---|---|---|
| Borderline | 100% | 90% |
| Malignant | 70% | 25% |
Table 2: 5-year survival of each histologic grading and staging 1
Reference
- Robbins & Cotran Pathologic Basis of Disease 10th Edition, chapter 22, page 1017-1020
- https://www.pathologyoutlines.com/topic/ovarytumorserouscarcinomahg.html
- Mallen, A.R., Townsend, M.K., & Tworoger, S.S. (2018). Risk Factors for Ovarian Carcinoma. Hematology/oncology clinics of North America, 32 6, 891-902 .
- https://www.pathologyoutlines.com/topic/ovarytumorserousbenign.html
I am currently just a final year med student, this is my study note and is not intended as medical advice. The content may contains inaccurency